the MOST®
The Memory Orientation Screening Test (the MOST®) is a short, easy to administer, highly reliable, and valid measure of cognitive functioning for patients.


Rapid, Accurate, Reliable
The Memory Orientation Screening Test (the MOST®) is a well-developed, extensively researched, often used, but not well-known measure of cognition that can be the brief go-to test of cognitive status across many different settings. The MOST correlates very highly with 4-hour batteries of neuropsychological tests involving measures of intelligence, attention, memory and executive function.
The MOST accurately identifies Mild Cognitive Impairment (MCI) and dementia, separating them efficiently from cognition that is normal for age.
The MOST is highly reliable and reflects stability or change in cognition over time.
The MOST is easy to use, well-accepted by patients at all levels of cognition, easily translated into foreign languages, uses universal stimuli, and can be administered electronically in person or over digital media.
Simply put, it is the MOST®.
The MOST® BASICS
Composed of 4 elements:
M emory for three words
O rientation to date and time
S equential recall of 12 pictured household objects
T ime organization and hand setting on a predrawn clock (optional animal naming)
- – Five minutes to administer and score
- – 0-29 point scale, higher scores reflecting better cognition
- – Hand or computer administration and scoring
- – In person or over digital media
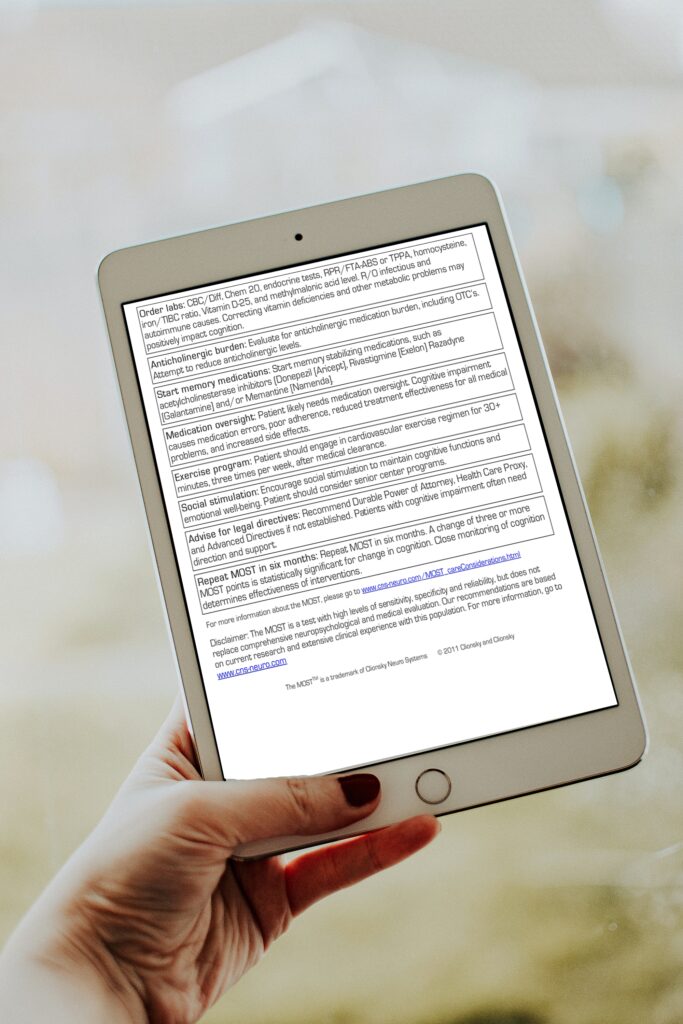
- – Generates a professional report for diagnosis and care
- – Level of cognition: normal vs. MCI vs. mild/moderate/severe dementia
- – Subsequent diagnostic steps to pursue
- – Labs, Scans, PSG, other tests or referrals
- – Medications to consider
- – Lifestyle interventions to consider
- – Generates a patient/family report, in accessible language and action steps
- – Modifiable for applied settings or research
The MOST® Key Features
click (+) to expand
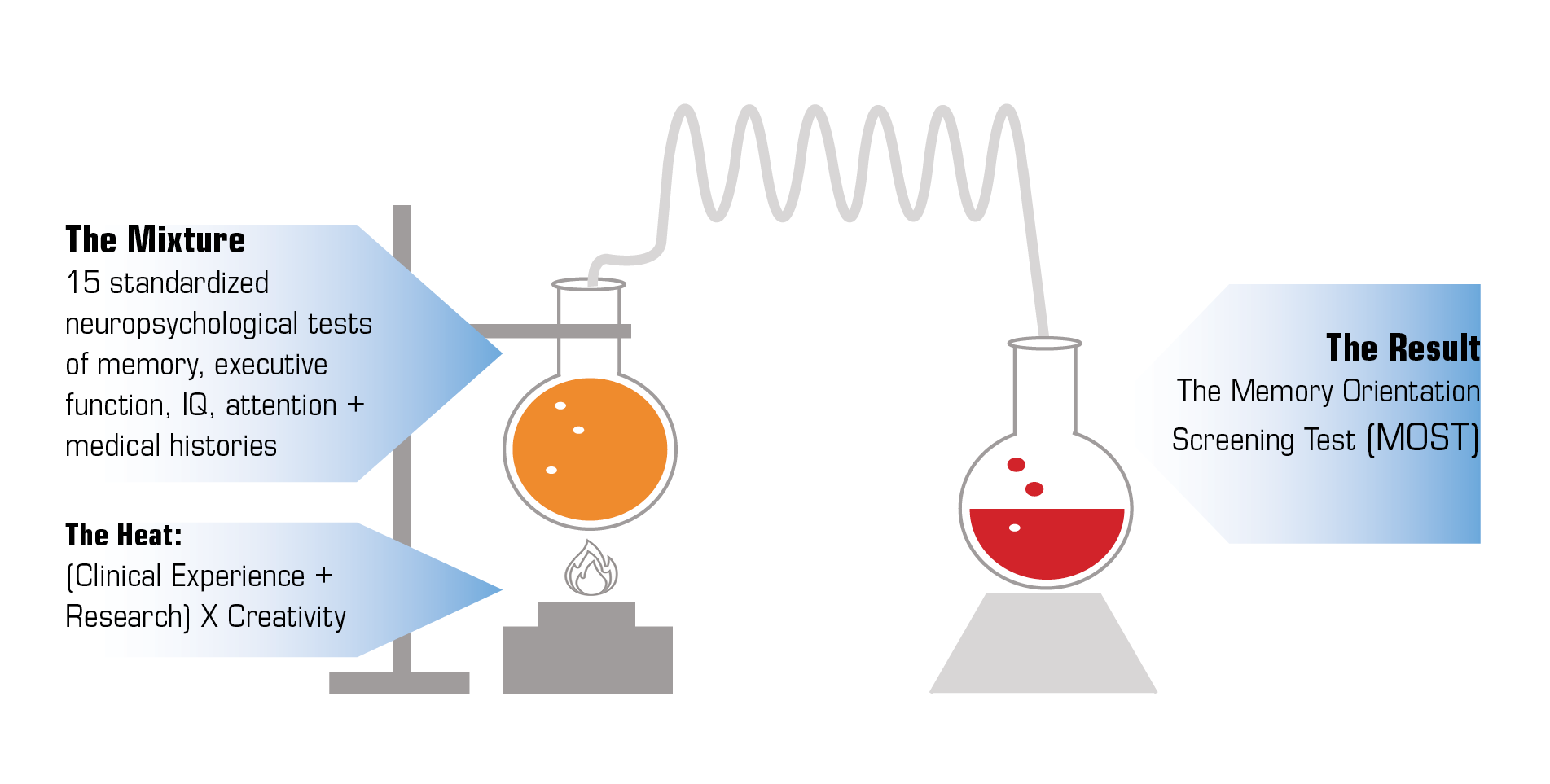
Distilling It All Down
When 15 standardized neuropsychological tests are distilled down with clinical experience and research the end result is the essence of all neuropsychological testing, The Memory Orientation Screening Test (the MOST®).
Concentrated:
3½ hours of testing in five minutes
Powerful:
r >.80 with dementia severity 88% sensitivity, 83% specificity
Stable:
r >.90 over one year
Portable:
iPad app
Easy to use:
From test to report in minutes No special training required
Accurate. Versatile. Economical.
PUBLISHED STUDIES: ACCURACY and RELIABILITY of the MOST®

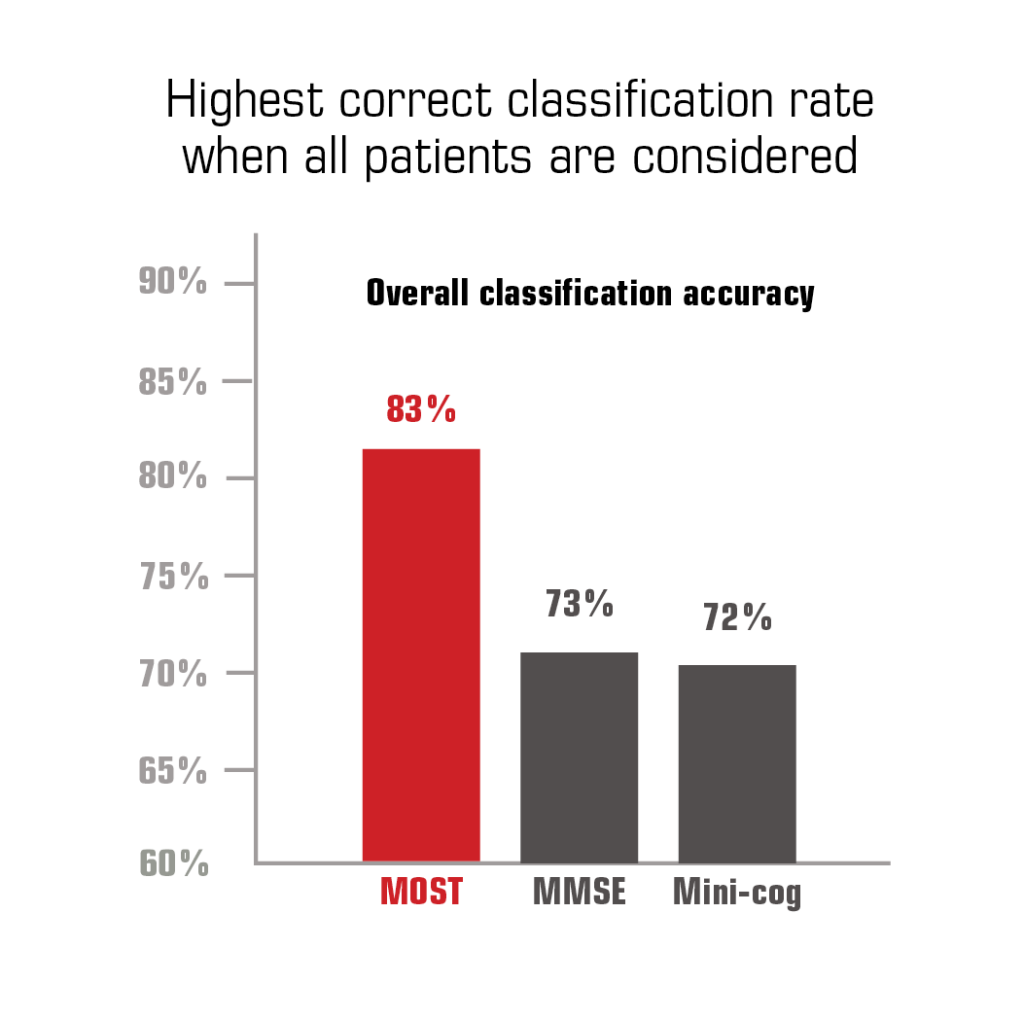
Development and validation study: Demonstrated brevity, accuracy, and comparative advantage over existing brief screening tests on a sample of 1752 memory clinic patients. 1
Results: The MOST was significantly more sensitive than MMSE or Mini-Cog, twice as accurate as MMSE for identifying mild dementia, better correlated with standardized memory tests, more reliable over time, and minimally related to depression.
Conclusions: The MOST is routinely administered in less than 5 minutes by a medical assistant, more accurately identifies dementia and severity than current screening tests, and emulates longer memory testing, making it valuable for Annual Wellness Visits and many applied clinical settings.

The MOST showed very high (r = .86) correlation with dementia severity and outperformed MMSE, patient and family ratings on sample of 201 patients. 2
Abstract conclusion: This study found that patients, family members, and even physicians have trouble detecting cognitive impairment. A better bet: Routinely administer an objective cognition test.

The MOST showed 80% correct diagnostic classification on US population prevalence-stratified (normal vs MCI vs dementia) sample of 217 elders. 3
Results: The MOST correlated highly with diagnostic severity and each neuropsychological test, demonstrating 80% correct diagnostic classification. The MOST showed a stronger relationship with dementia severity and list memory than MMSE. MOST cutting scores provided 88% sensitivity and 83% specificity for identifying MCI and dementia, yielding a PPV of .72 and NPV of .93.
Conclusion: The MOST accurately classifies patients from a diagnostically proportioned sample as normal, MCI, or demented and has high sensitivity and specificity for separating normal from impaired. Providers can use this 5-minute test to accurately identify cognitively impaired patients and to reassure elders with normal cognition, while acknowledging that no single test is adequate for making a definitive diagnosis.

The MOST paper and iPad versions showed high equivalency and accuracy of diagnosis on 98 consecutive NP patients. Found no 1-hour repeat test practice effect. 4
Abstract conclusions: ANOVA showed no significant difference between versions or presentation order. Both versions correlated very highly with cognitive level and neuropsychological endpoints, confirming previous research. The MOST-96120 is a computerized neuropsychological assessment device that demonstrates equivalence with its paper-based original, allowing for confident reliance on the findings of previous research.
HISTORY
The Future of the MOST®
click (+) to expand
Are you interested in the MOST®?

Yes, I am a corporation that is interested in partnering with CNS regarding the MOST.
Please contact us to discuss possible partnership opportunities.
1 Clionsky, M and Clionsky, E, “Development and Validation of the Memory Orientation Screening Test, American Journal of Alzheimer’s Disease and Other Dementias, 2010, 25 (8), 650-656. doi: 10.1177/1533317510386216
2 Clionsky, M and Clionsky, E, “Identifying Cognitive Impairment in the Annual Wellness Visit: Who Can You Trust?” Journal of Family Practice, 2011, 60: 653-659.
3 Clionsky, M and Clionsky, E, “The Memory Orientation Screening Test (MOST) accurately separates normal from MCI and demented elders in a prevalence-stratified sample, Journal of Alzheimer’s Disease and Parkinsonism, 2013, 3:1, http://dx.doi.org/10.4172/2161-0460.1000109
4 Clionsky, M and Clionsky, E, “Psychometric Equivalence of a Paper-Based and Computerized (iPad) Version of The Memory Orientation Screening Test (MOST), The Clinical Neuropsychologist, 2014,
http://dx.doi.org/10.1080/13854046.2014.913686